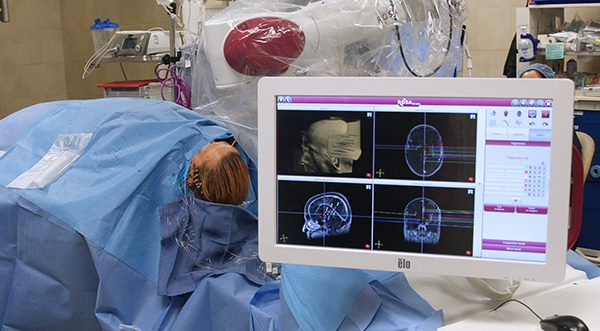
In August 2016, the Epilepsy and Movement Disorders Program at UPMC became the only program in western Pennsylvania to adopt the ROSA stereotactic robotic system for placement of electrodes in sEEG surgeries. We now routinely use ROSA for DBS, RNS, and LITT surgeries as well. ROSA reduces operating time by half or more and also improves surgical accuracy. Utilizing ROSA for electrode placement marks an important step towards safer and less invasive surgery for epilepsy and movement disorders. Being able to perform these surgeries through smaller openings in the skin and bone has led to improved patient comfort and outcomes.
ROSA is similar to a GPS device for the brain. The robot does not insert the electrodes or do anything directly to the patient, but it provides the surgeon with a roadmap to reach the intended brain targets. ROSA’s arm is engineered with 6-degrees-of-freedom, allowing exceptional dexterity and flexibility to access surgical sites for the rapid and precise alignment of multiple trajectories for electrode placement.