Epilepsy remains one of the most common neurologic disorders affecting both adults and children alike, and over two million individuals in the United States have this disease. Approximately 30% of patients with epilepsy are considered "medically intractable" meaning that they continue to have seizures despite treatment with medications. It is in this group of patients that seizures have the most significant impact on quality of life including relationships with family, friends and co-workers, and the ability to work and to drive. It is estimated that as many as half of these patients with medically intractable epilepsy would benefit from a diagnostic or therapeutic surgical procedure.
Surgical Candidacy
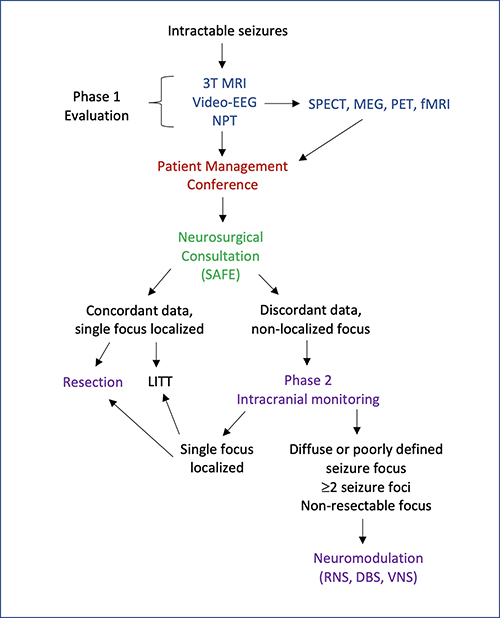
Patients with medically intractable epilepsy by definition have failed at least two antiepileptic medications, but patients have often been trialed on multiple medications for an unduly long period of time. The chance of being seizure free from medication alone after failing two appropriate seizure medications is extremely low. Severe medication side effects may also be an indication for surgery. In addition, anyone with tumor, vascular malformation or other brain lesion that is causing seizures should be evaluated by an epilepsy surgeon. To determine if a patient is a candidate for epilepsy surgery, an extensive evaluation is undertaken, including video-EEG, anatomical (MRI) and functional (PET, SPECT, MEG) imaging, and neuropsychological testing. This initial, non-invasive “Phase I” evaluation provides a comprehensive overview of the seizure syndrome.
Surgical Treatment
Stereo-EEG
Some patients require no further testing and go on directly to surgery. The type of surgery is based on the epileptic syndrome, imaging and electrophysiological findings. For other patients, non-invasive testing fails to pinpoint the exact seizure focus, and additional monitoring is required before proceeding with surgery. For these patients, a diagnostic surgery called sEEG may be necessary to further define the seizure focus.
SEEG is the surgical implantation of electrodes into the brain in order to better localize the seizure focus. At UPMC, we use robotic assistance with ROSA® to accurately and efficiently place the electrodes for seizure mapping. Jorge Gonzalez-Martinez, MD, PhD, was the first epilepsy surgeon in the US to offer SEEG and has performed over 1000 cases. He is also a pioneer of robotic-assisted neurosurgery, which improves accuracy and shortens surgery time.
The electrodes are implanted in the operating room and then the patient is monitored in the Epilepsy Monitoring Unit (EMU) for about a week (sometimes longer) to record seizures. The electrodes can also be stimulated in order to identify important functional areas of the brain such as the language center. These data are reviewed by the entire epilepsy team, and a recommendation for surgery may be made based on these result.
Craniotomy for Resection of the Seizure Focus
Epilepsy surgery typically consists of a resective procedure, which is most likely to result in a cure since the goal is to excise the seizure focus itself. The most common type of resection is an anterior temporal lobectomy. Outcomes following resective surgery for the treatment of epilepsy have markedly improved over the last few decades. For patients with temporal lobe epilepsy, it is now widely accepted that surgery is superior to prolonged medical therapy. Frequently with this type of surgery, the proportion of properly selected patients who are seizure free after surgery can be above 70%. While the other types of resective surgery are less likely to have a seizure free outcome, the numbers are proportionately better than medical therapy alone. Seizure free outcomes range from 30- 70% for surgery outside the temporal lobe.
Laser Ablation
In 2015, our epilepsy program became the first in western Pennsylvania to offer laser interstitial thermal therapy (LITT) as an alternative to surgical resection of a seizure focus. LITT is a procedure, like open resection, that may potentially cure a patient’s epilepsy. Rather than removing it, however, the seizure focus is ablated using heat generated from a laser at the tip of a very thin probe. This minimally invasive procedure is performed through an incision about the width of a pencil’s eraser and most patients are discharged home within 1 day.
Responsive Neurostimulation (RNS®)
In 2013, the FDA approved the use of responsive neurostimulation (RNS) in the treatment of adults with medically refractory focal onset seizures arising from one or two foci in the brain. RNS is a long-awaited treatment for a large group of patients who were previously determined not to be candidates for epilepsy surgery, such as patients with multifocal epilepsy or with seizures arising from areas of the brain that cannot be safely resected. Although this surgery is unlikely to be curative like surgical resection, RNS has been shown to reduce seizure frequency by ~68% at 1 year, and seizure reduction continues to improve with time.
Deep Brain Stimulation (DBS)
DBS is a brain stimulator that has been used to treat movement disorders since the 1990s. It has been more recently approved to treat intractable epilepsy. DBS has been shown to reduce seizure frequency by 41-56% 1-2 years after surgery, and the seizure reduction continues to improve with time. It is indicated to treat patients with medically intractable epilepsy who are not candidates for resection of their seizure focus.
Vagus Nerve Stimulation (VNS)
Vagal nerve stimulator (VNS) has been shown to reduce seizures by half or more in about 40% of patients 1 year after surgery and seizure reduction continues to improve with time. It is indicated for patients with medically intractable epilepsy who are not candidates for other types of surgical intervention. The device consists of a wire that is wrapped around the vagus nerve in the neck and a battery that is placed in the chest. VNS does not stimulate the brain directly and this surgery can be performed as an outpatient.
Others
Other less commonly used surgeries including multiple subpial transections (MST), corpus callosotomy, and others are available to patients who may benefit from them. These surgeries are palliative rather than curative since they do not eliminate the seizures but interrupt the propagation of the seizures. Despite that, these procedures can improve the patient's quality of life by decreasing the frequency and intensity of the seizures.
Future Options
The utility of epilepsy surgery is likely to continue to grow in the future, since the majority of patients who are potential surgical candidates have not been evaluated and treated. It is estimated that less than 3% of patients who would benefit from a surgery actually undergo treatment. With improved awareness of the benefits of surgery and ongoing technological advances, surgery for epilepsy is now well-established and readily identified as the optimal therapy for many forms of intractable seizures.
Cutting-edge, minimally invasive, and personalized approaches are a cornerstone of the epilepsy surgery program within the UPMC Comprehensive Epilepsy Center, the only such comprehensive program in western Pennsylvania. Individuals with recurring seizures, their families, and/or their physicians, are encouraged to contact the program for more information regarding the modern standards of diagnostic and therapeutic epilepsy care.
