In 2015, UPMC Presbyterian became the first hospital in western Pennsylvania to perform laser ablation (also known as Laser Interstitial Thermal Therapy, or LITT) for epilepsy. LITT is a procedure, like open resection, that may potentially cure a patient’s epilepsy. Rather than removing it, however, the seizure focus is ablated using heat generated from a laser at the tip of a very thin probe. This minimally invasive procedure is performed through an incision about the width of a pencil’s eraser and most patients are discharged home within 1 day.
How is LITT performed?
At UPMC, we use the Monteris NeuroBlate® System for LITT via an interventional-MRI approach. Procedurally similar to the placement of depth electrodes during sEEG, we use ROSA robotic assistance to insert the laser probe. Then, the ablation itself occurs under MRI guidance. Special MRI scans are used to report the temperature of the target tissue and to create a continuous visual representation of the ongoing ablation. In mesial temporal lobe epilepsy, for instance, the ablation is confined to the hippocampus and amygdala, without affecting adjacent brain tissue (see image below).
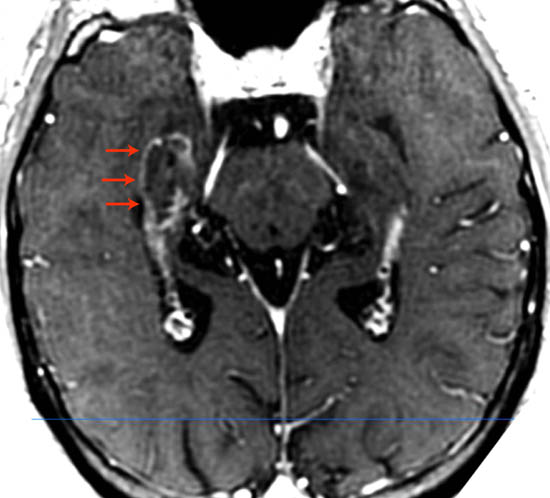
Above is a postoperative MRI image demonstrating selective ablation of the hippocampus. The contrast-enhancing border of the ablated tissue is delineated with red arrows.
Who is a candidate for LITT?
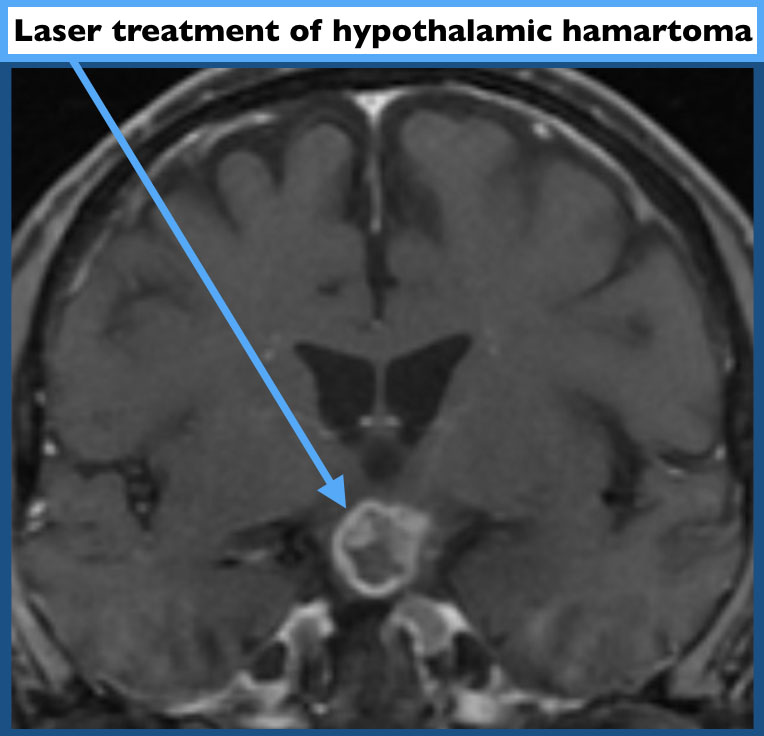
Patients who have had a thorough work up through our comprehensive epilepsy center may be offered LITT once we have localized their seizure focus to a well-defined area. These patients may have temporal lobe epilepsy with an MRI finding of mesial temporal sclerosis (MTS), or they may have a seizure focus in another brain region that has been well pinpointed by sEEG. We also offer LITT as a treatment for seizures caused by a hypothalamic hamartoma. LITT also can be used to treat a variety of brain tumors in patients with or without epilepsy.